Treatment for Epithelial Cancer of the Ovary at Gleneagles Hong Kong Hospital (GHK) – The GHK Experience
Overview of ovarian cancer
According to data from the Hong Kong Cancer Registry, cancer of the ovary is the sixth commonest female cancer and ranks second for gynaecological cancer. In 2017 in Hong Kong, 651 patients were diagnosed to have cancer of the ovary.
Unlike cancer of the cervix with the Pap smear, there is no effective screening test for early or pre-cancer of the ovary. In the early stage, cancer of the ovary is usually asymptomatic. When symptoms appear, they are vague and can be confused with other common conditions. Some symptoms may include abdominal distension, abdominal discomfort and easy satiety.
At initial presentation, 3 of 4 patients with ovarian cancer are already Stage III/IV. At this time, there is already spread of cancer to the abdominal peritoneum causing accumulation of fluid (ascites). These disturb the bowel function and hence the presenting symptoms of abdominal distension, abdominal discomfort and easy satiety. A provisional diagnosis of cancer of the ovary is made based on an elevated blood tumour marker (CA 125) and ultrasound, CT scan or MRI of the abdomen showing enlarged ovarian tumours, peritoneal spread of disease and presence of ascites.
It is at this juncture that the patient will be referred to a Gynaecological Oncologist with a provisional diagnosis of cancer of the ovary. It is the responsibility of the Gynaecological Oncologist to come to a definitive diagnosis and plan the patient’s subsequent treatment.
In Gleneagles Hospital Hong Kong (GHK), the Gynaecological Oncologist is supported by a multi-disciplinary team consisting of gynaecological oncologists, clinical oncologists, surgical oncologists, medical oncologists, radiologists and pathologists. This multi-disciplinary team of doctors constitute the Gynaecological Oncology Tumour Board. Since the inception of the hospital, the Gynaecological Oncology Tumour Board has met regularly and the 28th meeting was held on 5th October 2020. This meeting is open to all doctors interested in the management of gynaecological cancers.
The Gynaecological Oncology Tumour Board meets to consider the latest evidence-based treatment for patients with gynaecological cancers, to see which of these treatments and procedures can be safely and effectively applied to patients with gynaecological cancers at GHK. The speed of advance in cancer care is such that the team needs to be up to date with the latest research, and the full arsenal of available surgery, chemotherapy, targeted therapy and other proven treatments can be considered for patients at GHK.
The Gynaecological Oncology Tumour Board also discusses all patients with gynaecological cancers operated on in GHK, to ensure that patients are receiving the most appropriate care. This also serves as an audit and check on the treatment provided by all doctors accredited to perform gynaecological cancer procedures in GHK. To our knowledge, it is the only private hospital in Hong Kong to have a dedicated, regular meeting of the Gynaecological Oncology Tumour Board for this purpose.
The multi-disciplinary nature of the Gynaecological Oncology Tumour Board ensures that the combined experience of the members of the team are utilised in the management of every patient with gynaecological cancer in GHK. The open and frank audit of the management of patients ensures quality assurance for patients at GHK. It is a key tenet of GHK’s partnership with The University of Hong Kong to build, promote and implement strong clinical governance at GHK.
Since the advent of the Gynaecological Oncology Tumour Board, other surgical disciplines at GHK have also started regular tumour board meetings for their respective specialties at GHK as the benefits and advantages of a multi-disciplinary team approach for the management of complex cancer cases are seen.
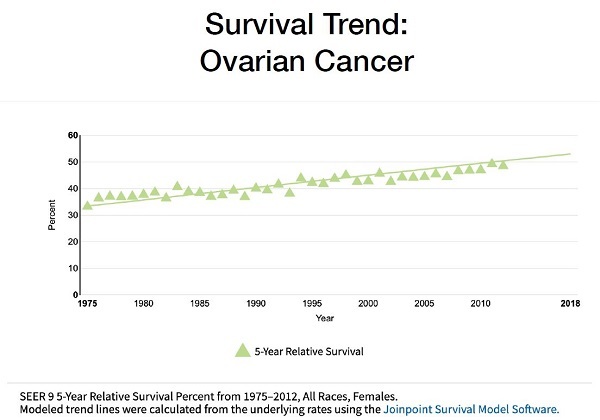
The mainstay of treatment for advanced stage ovarian cancer is surgery and chemotherapy with or without targeted therapy. With the recent advances in the management of epithelial ovarian cancer including appropriate use and timing of surgery, HIPEC, targeted therapy, maintenance therapy and other newer treatment modalities, we continue to see an improvement in survival rates of advanced epithelial ovarian cancer, as the above chart shows. In the best scenarios when patients are managed at dedicated centres of excellence, we are seeing 5-year relative survival rates of 60% to 70% compared to 20% to 30% a few decades ago.
One of the most important indicators of survival is how well the surgical team is able to remove all visible tumours from the peritoneal cavity. Research has shown that the difference between leaving no macroscopic tumour behind vs leaving 1-10mm tumour nodules behind is an improvement of 46.9 months in median survival if no visible tumour is left behind (Bristow, 2002). Hence the importance of the multi-disciplinary team decisions on selecting the most appropriate surgical management for the individual patient, to decide which patient would benefit from primary debulking surgery, or which patient is better suited to have chemotherapy first (neoadjuvant chemotherapy) to shrink the tumours before an attempt at interval debulking surgery. To this end, the team considers all the available clinical information including imaging (Ultrasound, CT, MRI, PET-CT). Often, a laparoscopic staging procedure is arranged to obtain histological diagnosis and evaluate whether patient is more suitable for a primary or interval debulking. The criteria and scoring systems for making this important decision is constantly being fine-tuned as new evidence comes to light.
The laparoscopic staging procedure through a single umbilical incision is an important first step in the management of a patient with suspected cancer of the ovary. The choice of laparoscopy and a single incision allows rapid healing and recovery of the patient so she can quickly go on to the next phase of treatment. Apart from making a definitive histological diagnosis of ovarian cancer, the laparoscopy allows the team to evaluate the stage and location of disease. Based on various scoring systems, a decision is then made whether the patient is suitable for primary debulking surgery or more suited to neoadjuvant chemotherapy and interval debulking surgery.
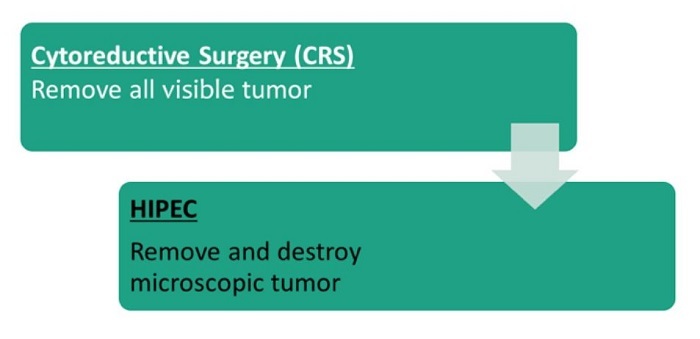
Regardless of the scoring system used, the crucial question to answer is whether the surgical team is able to completely debulk the patient to no visible disease at primary debulking surgery. If the answer is yes, she is planned for primary debulking surgery with or without HIPEC. If the answer is no, she is planned for neoadjuvant chemotherapy and interval debulking surgery with or without HIPEC.
The decision is highly individualised and is based on the team’s assessment of the patient’s general health, the final staging and histology of the tumour, the location of the tumour and whether it is suitable for successful primary debulking surgery to no visible tumour. For example in a patient with poor general condition and co-morbidity with a higher surgical risk, the team may consider neoadjuvant chemotherapy to shrink the tumour first so that a less radical interval debulking surgery with lower surgical risk could be done.
On the other hand, in an otherwise fit patient, the decision is made for neoadjuvant chemotherapy because of extensive tumour nodules on the small bowel and mesentery as complete resection of small bowel is incompatible with survival. These are just two of the permutations that the multi-disciplinary team need to consider when coming to an individualised decision for every patient.
Surgery for advanced stage epithelial ovarian cancer has continued to make progress over the years. Newer techniques and instruments together with greater collaboration between gynaecological and surgical oncologists means surgical teams are getting better at achieving optimal debulking which ideally is the complete removal of all visible tumour.
To further enhance the effect of a successful optimal debulking, the use of Hyperthermic Intraperitoneal Chemotherapy (HIPEC) at the completion of surgical debulking has gained traction over the years. The use of HIPEC came about as a logical evolution of what Gynaecological Oncologists have achieved in continuing to improve the survival of patients with advanced epithelial ovarian cancers.
Chemotherapy is conventionally administered intravenously. However, carcinoma of the ovary is by and large an intraperitoneal disease. Therefore when chemotherapy is administered intravenously, only a small proportion of chemotherapy drugs cross the peritoneal plasma barrier to reach the peritoneum where the ovarian cancer cells are. A more logical way of administering chemotherapy would be to give the chemotherapy directly into the peritoneal cavity (intraperitoneal chemotherapy).
In fact studies have shown that administering chemotherapy intraperitoneally increases the survival by 16 months compared to conventional intravenous chemotherapy. However, in practical terms, postoperative intraperitoneal chemotherapy is associated with side-effects, catheter blockages, patient inconvenience and postoperative adhesions which may hamper the distribution of chemotherapy evenly in the peritoneal cavity to reach the whole peritoneal cavity. Therefore the use of intraperitoneal chemotherapy was not as widespread despite its survival advantages.
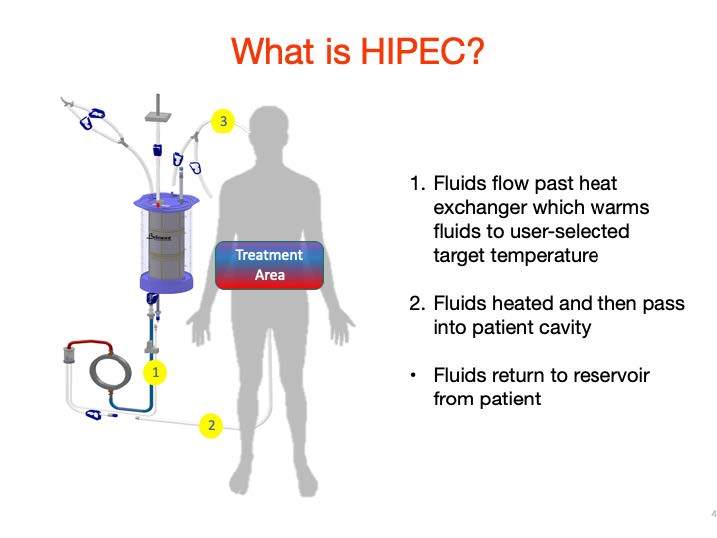
HIPEC is intraperitoneal chemotherapy administered at the time of surgery after successful complete debulking surgery. In GHK, we use the closed technique. Essentially, at the end of successful complete debulking surgery, the patient’s abdomen is temporarily closed. While still under anaesthesia, two tubes are in place in the peritoneal cavity connected to a machine outside. The machine heats the chemotherapy drug, in this case cisplatin at a dose calculated for the patient to a temperature of 42°C and then pumps the chemotherapy drug into the peritoneal cavity through one tube. An adequate volume ensures that the whole of the peritoneal cavity is bathed in this chemotherapy solution. The other tube is the outflow from the peritoneal cavity back to the machine. In this way, the chemotherapy drug is continuously circulated to bath the peritoneal cavity at a set temperature of 42°C for 90 minutes. At the end of this time, the abdomen is re-opened and surgery completed and patient is brought out of anaesthesia.
The advantages of HIPEC are:
- Heat increases drug penetration into tissue
- Heat has anti-tumour effects by itself
- Heat increases cytotoxicity of the selected chemotherapy agents
- Intraperitoneal Chemotherapy assure a high concentration of anticancer therapy at the peritoneal surfaces
- Intraperitoneal Chemotherapy can overcome peritoneal-plasma barrier
On January 18, 2018 a landmark study was published in the New England Journal of Medicine. This was a prospective randomised trial which showed that the addition of HIPEC to interval debulking surgery conferred a 12 months increase in overall survival compared to surgery alone. On January 31, 2018, the team at GHK performed the first HIPEC surgery for ovarian cancer in Hong Kong.
At GHK, chemotherapy is administered by clinical or medical oncologists. Upon completion of chemotherapy, suitable patients are offered maintenance treatment, which may consist of oral targeted therapy to decrease the chance of recurrence.
The last few years has seen rapid advances in the care of women with advanced stage ovarian cancer. Compared to 30 years ago when the 5-year survival rate was 20% to 30% in this group of women, we are now seeing relative 5-year survival rates approaching 70% in selected women with appropriate treatment.
At GHK, our multidisciplinary team in Gynaecological Oncology are committed to offering the best evidence-based treatment for our women with ovarian cancer. Our priority is to ensure that our patients receive the safest and most cost-effective care. Working together and taking full advantage of the combined experiences of our multidisciplinary team members, we are committed to providing the most appropriate and innovative care for our patients.
Mrs. Chan, 56 years old, consulted her General Practitioner (GP) for abdominal discomfort and distension worsening over the past 3 weeks. She reported a sensation of feeling full after eating only a small amount (easy satiety). She had menopause at 52 years old and had no abnormal vaginal bleeding since. Her urinary and bowel habits were normal. She had a normal gynaecological examination including Pap smear and pelvic ultrasound two years ago.
Her GP did a careful examination and found that her abdomen was moderately distended with fluid (ascites). An abdominal ultrasound was ordered and this showed moderate ascites and an 8 cm right adnexal mass suspicious for ovarian cancer. She was then referred back to her regular gynaecologist for assessment.
Her gynaecologist confirmed the above findings. Tumour markers CA 125 and CEA were done. CEA was normal but CA 125 was markedly elevated to 600 U/ml. A CT scan of the abdomen and pelvis was arranged. This showed massive ascites with multiple irregular enhancing peritoneal and omental masses suggestive of peritoneal malignancy, more likely secondary rather than primary. A complex mass was seen in the right adnexal region suspicious for primary ovarian cancer. A provisional diagnosis of ovarian cancer was made.
She was then referred to see a gynaecological oncologist for further management.
Mrs. Chan was seen by a gynaecological oncologist at GHK’s Specialist Outpatient Clinic. Her history was reviewed, an examination done and CT scans reviewed. After clinical evaluation, a provisional diagnosis of Stage III carcinoma of the ovary was made and the treatment plan discussed with Mrs. Chan.
The gynaecological oncologist gave an overview of ovarian cancer and how it spreads in the peritoneal cavity. It was explained that the next step was to obtain a histological confirmation of her diagnosis of ovarian cancer. The role of surgery and chemotherapy with or without targeted therapy was also discussed.
In particular, the role of surgery in obtaining a histological diagnosis and for the removal of all visible primary and metastatic ovarian cancer in the peritoneal cavity was emphasised. It was also explained that if it was judged that a complete removal of all visible tumour was not possible (primary debulking), there was the option of using chemotherapy to shrink the tumour first (neoadjuvant chemotherapy) before surgery is done to remove all visible tumour at a later stage (interval debulking).
The addition of Hyperthermic Intraperitoneal Chemotherapy (HIPEC) at the time of debulking surgery to enhance the effects of the surgery and to improve results was also discussed. Other modalities of treatment including targeted therapy and maintenance therapy was also discussed at this juncture. Mrs. Chan was given ample opportunities to ask questions. She was also invited to take some time to process all the information she had been given, and to discuss with her family and significant others before coming to a decision on treatment.
Information sheets and web resources on cancer management was given to Mrs. Chan. A Fee Advisory was arranged to discuss the expected costs of the surgery and treatments proposed so Mrs. Chan and her family had a clear understanding of the estimated total costs involved.
After discussing with her family, Mrs. Chan decided to follow the recommendation of the gynaecological oncologist to have a laparoscopic staging procedure to obtain a histological diagnosis of cancer of the ovary as well as to evaluate whether she is suitable for primary debulking or interval debulking after neoadjuvant chemotherapy.
A single incision laparoscopic staging procedure was done for Mrs. Chan. This was performed through a single umbilical incision. After removing the ascitic fluid which was sent for cytological examination, a thorough evaluation of the peritoneal cavity was made, mapping the location and size of all visible lesions. The right adnexal mass was removed surgically and retrieved through the umbilical incision. The bulk of tumour on the omentum was similarly removed. It was noted there were peritoneal seedlings of tumour on the peritoneum, as well as tumour seedlings on the small bowel. A laparoscopic staging procedure, debulking of tumour and biopsy was done.
Cytological examination of the ascitic fluid was positive for malignant cells. Histology of the right adnexal mass and omental tumour showed High Grade Serous Carcinoma of the Ovary. Mrs Chan had Stage IIIC High Grade Serous Carcinoma of the Ovary.
Mrs. Chan was seen with the results of her laparoscopic staging procedure. Because of the extensive tumour nodules on the small bowel and mesentery, she was not suitable for primary debulking surgery. The decision was made for neoadjuvant chemotherapy and then consideration for interval debulking surgery with or without HIPEC later.
Mrs. Chan was evaluated by the Clinical Oncologist/Medical Oncologist who would be responsible for her chemotherapy. The procedure of administration, side-effects of the proposed chemotherapy: carboplatin and paclitaxel were discussed. The utility of somatic and germline mutation testing of her cancer cells for BRCA mutation and its impact on maintenance therapy after completion of treatment was also discussed.
Once her Gynaecological Oncologist had evaluated Mrs. Chan’s postoperative recovery and pronounced her fit for chemotherapy, she was started on her 3 weekly cycle of carboplatin and paclitaxel. Her treatment decisions and plans were also discussed at the Gynaecological Oncology Tumour Board to arrive at a consensus for her treatment.
Mrs. Chan successfully completed 3 cycles of neoadjuvant chemotherapy consisting of carboplatin and paclitaxel every three weeks. She had minimal side-effects and tolerated chemotherapy well. Her tumour markers CA 125 decreased to a normal level (<35 U/ml). A PET- CT scan was done. This was compared to her pre-treatment PET-CT and there was marked improvement with resolution of most lesions in the peritoneal cavity.
After evaluation by her gynaecological oncologist, she was scheduled for an interval cytoreductive surgery and HIPEC. The procedure and risks were discussed with her. An admission was arranged for surgery and HIPEC which was done successfully. She recovered well from her surgery and was referred back to her oncologist for completion of her chemotherapy.
Upon completion of her chemotherapy, her oncologist will also discuss with her newer targeted therapies which can decrease the chance of recurrence of her ovarian cancer.
Enquiries/Appointments:
+852 3153 9153 (Obstetrics & Gynaecology Clinic)